Join The 80%: CBCT And Endodontics
Nestor Cohenca, D.D.S., FIADT
2/26/2023
Based on a study published by Setzer et al., in 2017 at the Journal of Endodontics, 80.3% of endodontists have access to a CBCT; 50.69% have the technology on-site and 49.31% have access to the technology off-site. The technology has proven essential in many fields of dentistry and we’ve come a long way since large, complicated imaging systems were relegated to universities and reserved for only the most complicated cases. Today, systems are smaller and more capable of meeting the unique needs of endodontists than ever before, making a CBCT system something to consider for your practice and your patients.|
A Brief History of the CBCT and Endodontics
Most of the major changes in endodontics, both in concepts and technology, started in the early 2000s. The use of microscopes, biological materials and rotary instrumentations were some of the most significant advancements in endodontics in the 21st century. Then came CBCT imaging. Initially used in academic institutions—mostly for trauma, root resorptions and pre-surgical assessment—CBCT imaging revolutionized the field. Doctors acknowledged the advantages, but most were reluctant to implement the technology due to its size and cost. It took a few years, but around 2009, with incentives given to graduate programs which led to further development, research and clinical experience, the technology developed exponentially. Part of that was fueled by the introduction of systems that were more affordable and with a relatively small footprint.
Wow’ Imaging for More Confident Diagnosis and Patient Confidence
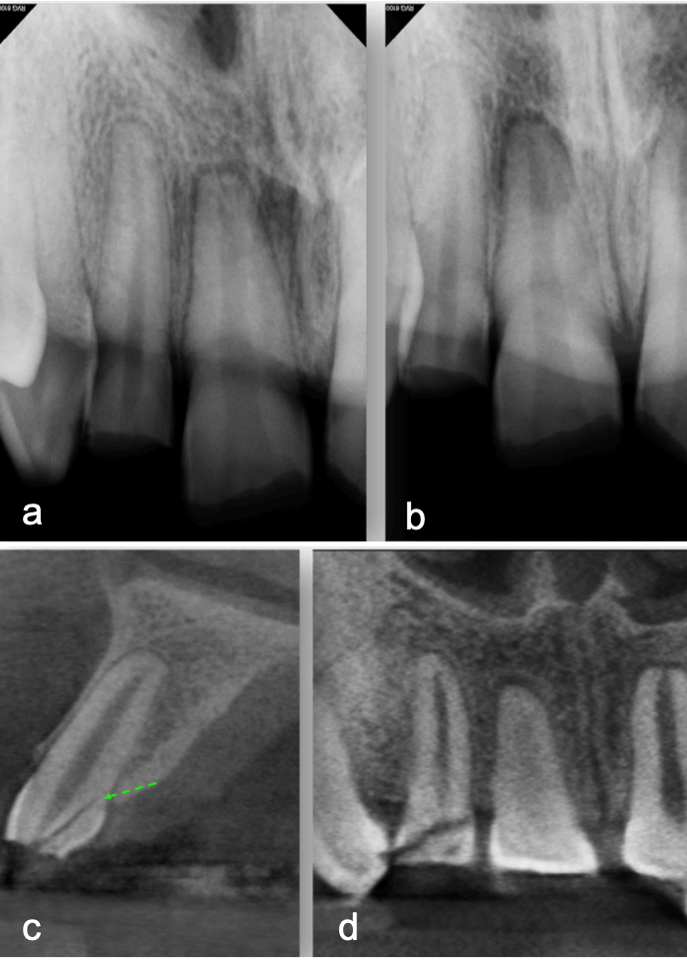
My first “wow” moment with CBCT was during the early years of the technology when scanning a patient after a traumatic dental injury that lead to lateral luxation of the maxillary left central incisor. The CBCT scan was able to produce images that previously had only ever been drawn or imagined. Those stunning 3D images have only gotten better over time. When indicated, 3D imaging provides critical information toward development of the best treatment plan. High-resolution images give endodontists the ability to change course and adapt quickly if needed to achieve better outcomes. Being able to diagnose a predictable failure also avoids unnecessary invasive procedures. For example, cases of root fractures or deep cracks (figure 1). For root canal retreatments understanding the etiology of the disease or failure is critical to obtain a positive outcome. CBCT also aids with enhanced visualization of traumatic injuries, particularly for crown, root fractures and luxation injuries (figure 2). Ultimately, the more accurate and realistic assessments of prognoses, the more predictable and positive outcome for my patients.
From the patient’s perspective, the “wow” moments happen daily when they can see their jaw and teeth moving three-dimensionally. More important, the fact that patients can now see exactly what’s the problem and understand the available treatment options is critically important to obtain an informed decision. Rather than trying different procedures with unpredictable results, CBCT imaging can save patients time, money and stress; for example, excluding unsavable teeth from the very start of the treatment plan. An additional benefit of CBCT imaging is differential diagnosis of chronic pain. Instead of prescribing medication to treat the symptoms, CBCT has the potential to instantly reveal the underlying problem allowing me to provide the correct treatment and relief.
Invest in Hardware, Reap the Benefit of Software
Today, CBCT imaging is driven by advanced software algorithms. That means that the software that powers these systems is just as important as the equipment itself. The quality of the 3D scans, the ease of use and the ability to share scans with referrals all come down to software. Ultimately, the hardware will not change much in the coming years; however, software updates and other new features and improvements must be pushed out by the manufacturer to ensure doctors are always practicing with the most advanced technology. Some examples of these updates can lead to improved image quality, digital measurements and reconstructions, metal artifact reduction (MAR) and therapeutic guides for surgical and non-surgical cases.
Spreading the Word about CBCT
If you’re still on fence about CBCT, why not experience it for yourself? Webinars, study clubs, trade shows and hands-on events give doctors every opportunity to explore their CBCT options. In fact, after setting up my new practice and installing a CS 8100 3D (Carestream Dental), I recently founded the Kirkland Study Club with the purpose of creating a multidisciplinary group of professionals willing to share and learn from each other. The first meeting covered a topic relevant to anyone looking to learn more about what CBCT could do for their patients and practice: “Clinical Applications of CBCT in Endodontics.” Upcoming meetings will cover topics such as advanced Invisalign concepts; immediate implant placement; non-invasive dentistry; keys to managing growth and eruption in the mixed dentition and more. Additionally, Carestream Dental makes it easy for doctors looking to get a sample of CBCT imaging at carestreamdental.com/3D with a digital library of 3D imaging resources. Studies and research show more and more the benefits of CBCT in endodontics, and 80% of the profession can’t be wrong. Join us on the other side with enhanced imaging, improved diagnosis and better patient care.
&srotate=0)
a-b. Periapical radiographs from different angles. Patient was referred for endodontic therapies on teeth 19 and 20 with apical lucencies consistent w
&srotate=0)
a-b. Periapical radiographs from different angles. Patient presented immediate after a traumatic injury to maxillary anterior teeth. Clinical and radi
Recent Posts
ToothSOS for emergency care of traumatic dental injuries
ToothSOS for emergency care of traumatic dental injuries
Regenerative Endodontics: What are the options for failed cases?
Regenerative Endodontics: What are the options for failed cases?
Maxillary mucositis and its correlation to endodontically treated teeth.
Prevalence of maxillary mucositis and its correlation to endodontically treated teeth